One symptom of stress may be that you start to fancy chocolate, a burger or other unhealthy, high-caloric “pleasure foods” to calm yourself down. While eating these foods can indeed help to reduce stress, you may become overweight and diabetic as a result. How can you break the loop between stress and overeating?
Stress and food intake
People usually change their eating behaviors when they perceive themselves to be stressed. Although 20% of people do not change eating behavior during stress, the majority does. Around 40% or more increase, and 40% or less decrease caloric intake when stressed.
This difference is related to body weight before the stress kicks in. It seems that people who initially are at the upper range of normal, or are overweight, are generally more inclined to increase weight when stressed, whereas those who are of normal or underweight are not. In people with a higher body mass index, insulin concentrations are typically higher. Insulin is needed to store fat, so the more insulin you have, the more fat you will accumulate.
Many people under stress prefer pleasurable or palatable foods. These are foods that are rich in sugar or fat and are rich in calories. The enhanced caloric intake occurs even when you are not hungry or have no need for these calories. They will therefore be stored, and add to your body weight.
The emotional brain
In order to understand how insulin and stress work together to increase caloric intake, we have to consider a particular part of the brain. This is the “emotional brain” and can be subdivided into three different layers. Together they mix emotions into behavior and provide the motivation to do the behaviors.
The highest level in hierarchy concerns two areas in the cortex of the brain. This is the part that is visible on the outside of the brain. The cortical part of the emotional brain is located in the “insula”. The insula provides “feelings”, based on what you have seen, heard, smelled, touched or tasted. Or based on what the inside of your body has sensed (gastrointestinal tract, organs, pain in the body). The insula integrates with another part of the cortex. This is the anterior cingulate cortex, which is part of the prefrontal cortex. The insula and cingulate cortex are important for “motivated behavior”.
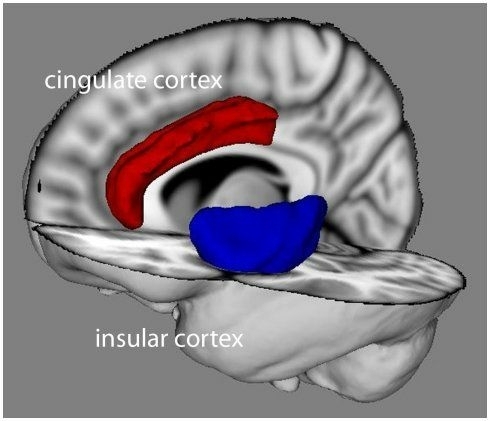 The cingular cortex (red) and insular cortex (blue) are part of the emotional brain. The face is to the left. From Anil Seth, Keisuke Suzuki and Hugo Critchley - Frontiers in Psychology, January 2012, Volume 2, Article 395.
The cingular cortex (red) and insular cortex (blue) are part of the emotional brain. The face is to the left. From Anil Seth, Keisuke Suzuki and Hugo Critchley - Frontiers in Psychology, January 2012, Volume 2, Article 395.
The cortical part of the emotional brain provides the consciously motivated output in response to what happens around you, and is based on how the “self” feels. This is thus the cognitive, or executive, component of the emotional brain, which can alter activity in lower brain regions.
The second level, below the cortical level, is the limbic brain. Here we find the hippocampus (memory), amygdala (emotion), nucleus accumbens (motivation) and the basal ganglia (habit). These brain structures operate all unconsciously, which is to say that you don’t have to think about them. They all work on autopilot. At this level, the amygdala is the site where emotions arise, and the nucleus accumbens provides motivation to carry out habitual behaviors appropriate to those emotions. As mentioned, the cognitive, executive control of emotions and drive is regulated by prefrontal structures (insula and prefrontal cortices).
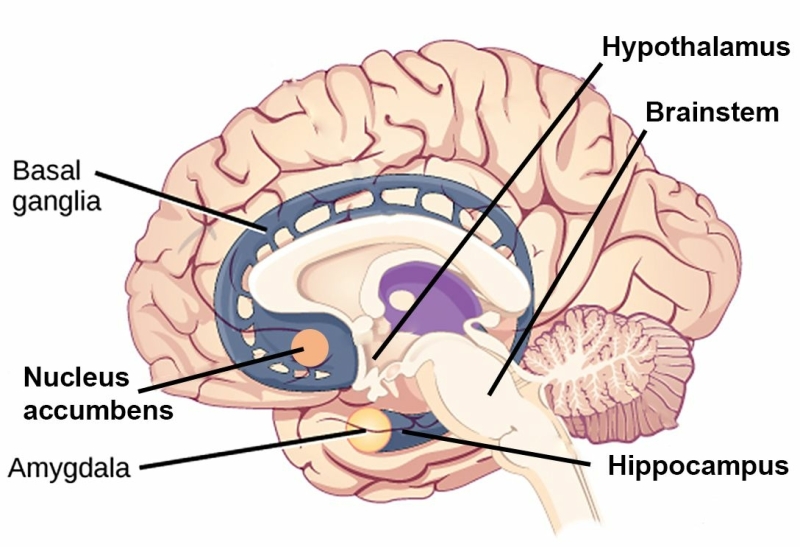 The basal ganglia, nucleus accumbens, amygdala and hippocampus are part of the limbic brain. The hypothalamus and brainstem form the lowest level of the emotional brain. The face is to the left. Adapted from CNX OpenStax through Wikimedia Commons.
The basal ganglia, nucleus accumbens, amygdala and hippocampus are part of the limbic brain. The hypothalamus and brainstem form the lowest level of the emotional brain. The face is to the left. Adapted from CNX OpenStax through Wikimedia Commons.
At the lowest level, we find the hypothalamus and the brainstem, which regulate energy balance, control anxiety and launch the reactions to stress. Regulation of energy balance serves to achieve equilibrium between how much energy your body needs and how much energy you have to consume to fulfill this need.
In summary, the emotional brain is composed of a conscious part, an unconscious part, and a regulating part based on actual needs.
Stress and the emotional brain
One of the hormones that is produced during stress is cortisol. It is the end product of the HPA-axis, which contains the hypothalamus with the protein CRF, the pituitary gland with the protein ACTH, and the adrenal glands that secrete cortisol into the blood.
One of the effects of cortisol in the brain is that it increases wanting or motivation. It does thus not decide which behavior you will adopt during stress, but it amplifies this behavior that is controlled by the unconscious part of the emotional brain, most notably the basal ganglia.
Cortisol also influences the conscious part of the emotional brain in the cortex. This leads to functional and structural changes, which decrease the ability to form memories, affect mood and are implicated in the development of depression.
Another important effect of cortisol is that it activates a stress-response system in the brain. This stress-response system is mediated by CRF, not in the hypothalamus but in the amygdala. The amygdala is the brain’s center of fear and part of the unconscious emotional brain. CRF is transported to other parts of the unconscious emotional brain and to the cortical, conscious part of the emotional brain. CRF is also transported to the brainstem where it activates, together with cortisol, the alert system.
The result of activating this stress-response system is that it overrides the negative feedback on the HPA-axis by cortisol. Negative feedback by cortisol makes sure that the activation of the HPA-axis stops after stress and the body returns to the normal, calm state. Overriding this shutdown mechanism ensures that the HPA-axis remains responsive to a new stressor. However, the stress response in the brain gives a stronger signal during chronic stress than the feedback signal, so that the stress does not stop.
Cortisol, food intake and insulin: “comfort foods”
Cortisol increases the motivation to increase caloric intake, probably by acting in the nucleus accumbens of the unconscious brain. This makes you eat more food that is rich in sugar or fat.
However, as mentioned earlier, cortisol does not make the selection to consume such “comfort foods”. It just increases the motivation of eating these. The selection is made under the influence of insulin. You may have heard of insulin as the hormone that brings sugar levels down in the blood. But it has turned out that it also has effects in the brain, working together with cortisol to select foods that are rich in sugar or fats.
Consumption of comfort food does indeed help to reduce stress responsiveness, which has been shown in rats. The production of CRF and ACTH in the HPA-axis is reduced when stressed rats are given the choice to eat fat or sugar instead of their normal chow. One could think that this effect of comfort food on the HPA-axis merely reflects a feeling of pleasure that reduces the discomfort of stress. However, comfort food does more than that. It also reduces the activity of the stress-response network by reducing the activity of CRF in the amygdala. It thus seems that a diet of hamburgers, washed away with coke, reduces the activation of the emotional brain during stress.
Cortisol, CRF, learning, memory and habit
Cortisol and CRF are important for learning and memory in the conscious and unconscious emotional brain. This is particularly true for events that provoke a negative emotion such as fear, and such events include the experience of stress. Therefore, when stress promotes the intake of comfort food through the actions of cortisol and insulin, memory is laid down for future recall for the stress-comfort food association. This is an association between “feeling stressed” and “feeling better” after indulging in “comfort foods”. Such an association may explain the link between stress and eating-induced obesity.
The association between stress and eating has yet another consequence, which is very important but is discussed only very little in programs aimed to reduce stress. Scientists have found that stress promotes the formation of habits at the expense of cognitive, goal-oriented behaviors. Habit formation typically occurs in the unconscious part of the emotional brain, in the basal ganglia to be precise.
What this means is that you are likely to transition from eating comfort food to feel better during intense stress to eating comfort food during mild stress without thinking about it. In other words, whenever you feel a little bit tense or tired, you will automatically reach out for a burger, fries, crisps and a bottle of coke to shake off stress.
There are two problems with the habitual use of comfort food to reduce stress. The first is, obviously, obesity. This is the consequence of greater sensitivity of abdominal adipose tissue to the combined signals from insulin and cortisol. The second problem is related to the loss of conscious thought about how to cope with a stressor (the thing that causes stress). Once stress-induced comfort feeding becomes a habit, the problem-solving, conscious part of the emotional brain (the anterior cingulate cortex) will underperform in dealing with stress. You may no longer be able to actively get rid of the stressor and comfort food intake becomes a reflex.
Being aware of what you do and what you eat
To reduce stress-induced eating of comfort food, it seems thus important to break the bad habits and to re-engage your conscious part of the emotional brain.
To achieve this, one could use mindfulness and meditation techniques, or consult a psychologist or psychiatrist, to train the cognitive, executive prefrontal brain (which includes the cingulate cortex) to overcome emotional, habitual eating. These techniques could help to become, be and remain aware of the nasty habits. As a result, you would become more likely to deal with the problem that gives you stress. Also, being aware of what you eat is a good thing in general, and could make you realize that you should spend more time in the kitchen cooking vegetables instead of quickly heating up a prepared meal from the supermarket.
Better still, you could enjoy good quality food in the presence of your family. Making dinner quality time devoted to your loved ones brings stress reduction again a step closer.
With that said, relieving an occasional strong stress by eating something pleasurable does not make you obese. It is perfectly OK to eat some chocolate to reduce stress once in a while. However, it is essential to not to engage in habitual relief of life’s discomforts by eating comfort, unhealthy, foods on a regular basis. This will inevitably lead to obesity and diabetes, and can even provoke premature death because of these.